Cataracts can develop for many reasons, but certain autoimmune conditions can increase your risk. Autoimmune diseases cause the body’s immune system to attack healthy tissues, and that inflammatory response can affect many parts of the body, including the eyes. When inflammation impacts the lens or the surrounding tissues, it can accelerate the development of cataracts.
Understanding the connection between autoimmune disorders and cataracts can help you protect your vision, seek timely care, and make informed decisions about your cataracts treatment. Here’s what you need to know.
How Autoimmune Diseases Affect the Eyes
The immune system plays a central role in defending the body from harmful pathogens. However, in autoimmune conditions, that same system misidentifies healthy cells as threats and begins attacking them. When this inflammation reaches the eye, it can damage the lens, cornea, or retina.
The lens, responsible for focusing light on the retina, is particularly sensitive. Chronic inflammation, immune cell buildup, and prolonged medication use, especially corticosteroids, can all contribute to cataract formation.
Corticosteroids are commonly prescribed to manage autoimmune symptoms. While they help reduce inflammation, long-term use has been closely associated with lens clouding. Both systemic (oral) and topical (eye drop) forms of corticosteroids can contribute to cataract development over time.
Autoimmune Conditions Commonly Linked to Cataracts
Several autoimmune conditions have been shown to increase the likelihood of developing cataracts. The following conditions represent some of the most frequent associations seen in clinical practice.
1. Rheumatoid Arthritis (RA)
Rheumatoid arthritis primarily affects the joints, but it can also lead to ocular complications. Chronic inflammation in RA can extend to the eyes, causing conditions such as scleritis and uveitis. Persistent eye inflammation can damage the lens and increase the risk of cataracts.
Additionally, individuals with rheumatoid arthritis often rely on corticosteroid medications to manage inflammation. Prolonged exposure to these medications is a well-known factor in cataract formation.
If you have RA, it’s vital to maintain regular communication between your rheumatologist and ophthalmologist. Regular eye examinations can help detect early lens changes before vision becomes affected.
2. Systemic Lupus Erythematosus (SLE)
Lupus is another autoimmune disorder that can affect nearly every organ system. Eye complications from lupus are not uncommon. Chronic inflammation can lead to damage to the cornea, retina, or blood vessels around the eye.
Patients with lupus are particularly vulnerable to cataract development because of both disease-related inflammation and medication exposure. Steroid therapy, a mainstay in lupus treatment, can accelerate cataract formation even at moderate doses when used for extended periods.
Monitoring for early visual changes such as glare sensitivity, hazy vision, or faded colors is key. These may be subtle indicators that cataracts are beginning to form.
3. Juvenile Idiopathic Arthritis (JIA)
Juvenile idiopathic arthritis affects children and adolescents, often involving the joints but sometimes extending to the eyes. Chronic uveitis is a common complication in JIA and can result in cataract development, particularly when inflammation persists or steroid eye drops are frequently required.
Because JIA patients may not notice early visual symptoms, regular eye check-ups are crucial. Detecting early lens changes allows for timely intervention before visual clarity is significantly affected.
4. Sjögren’s Syndrome
Sjögren’s syndrome primarily targets the body’s moisture-producing glands, leading to dryness in the mouth and eyes. Chronic dry eye increases discomfort and can heighten sensitivity to light, but over time, the inflammation associated with Sjögren’s can also influence cataract formation.
In addition to inflammation, long-term corticosteroid therapy used to manage systemic symptoms can accelerate lens clouding. Many individuals with Sjögren’s also have overlapping autoimmune disorders such as rheumatoid arthritis or lupus, which further raises their risk of developing cataracts.
Managing dryness with lubricating drops, maintaining hydration, and undergoing annual comprehensive eye exams can help minimize complications.
5. Type 1 Diabetes Mellitus
Although diabetes is primarily known as a metabolic disorder, Type 1 diabetes is autoimmune in origin. The immune system attacks the insulin-producing cells in the pancreas. Over time, this affects blood sugar regulation and can have direct consequences on the eyes.
Elevated blood sugar levels contribute to changes in lens metabolism, leading to clouding and cataract formation. Studies have shown that individuals with Type 1 diabetes tend to develop cataracts earlier in life compared to the general population.
Good blood sugar control, regular ophthalmic evaluations, and open discussion with your eye care provider about visual symptoms can help slow progression.
6. Multiple Sclerosis (MS)
Multiple sclerosis targets the central nervous system, disrupting communication between the brain and body. Although cataracts are not a direct symptom of MS, the disease’s treatment often involves long-term corticosteroid therapy to manage flare-ups.
Repeated or prolonged steroid exposure can result in posterior subcapsular cataracts, which form near the back of the lens. This type tends to affect reading vision and sensitivity to bright light.
For individuals living with MS, balancing treatment for neurological symptoms and eye health is key. Regular monitoring can help identify lens changes before they affect daily activities.
7. Uveitis Associated with Autoimmune Disorders
Uveitis, inflammation of the uveal tract, which includes the iris, ciliary body, and choroid, is often triggered by autoimmune conditions. Chronic uveitis is one of the most frequent ocular complications leading to cataracts.
Inflammation disrupts the transparency of the lens and may alter the composition of the lens fibers. Additionally, steroid medications used to control uveitis further contribute to lens opacity.
Autoimmune disorders most commonly linked to uveitis include rheumatoid arthritis, lupus, sarcoidosis, and ankylosing spondylitis. Managing uveitis effectively reduces the risk of cataract progression and preserves vision quality.
8. Sarcoidosis
Sarcoidosis is characterized by clusters of inflammatory cells forming in different organs, most often the lungs and lymph nodes, but it can also affect the eyes. Ocular sarcoidosis frequently leads to uveitis, which increases the likelihood of cataract formation.
Steroid use in sarcoidosis management compounds the risk. Both disease activity and treatment side effects may influence how soon cataracts appear.
Patients diagnosed with sarcoidosis should maintain consistent eye examinations even if they do not notice vision changes. Early detection can help guide timely management decisions.
9. Ankylosing Spondylitis (AS)
Ankylosing spondylitis is an inflammatory disease primarily affecting the spine and sacroiliac joints, but eye involvement is common. Up to 40% of individuals with AS experience anterior uveitis at some point, which significantly increases the likelihood of cataracts.
Repeated inflammation, combined with intermittent steroid treatment, sets the stage for lens changes. Prompt management of uveitis and ongoing follow-up with an ophthalmologist can reduce complications.
10. Psoriatic Arthritis
Psoriatic arthritis occurs in individuals with psoriasis and causes joint inflammation that mirrors aspects of rheumatoid arthritis. Eye inflammation is a less frequent but well-documented manifestation.
Prolonged systemic inflammation and steroid exposure can result in cataracts. Maintaining stable disease control through appropriate therapy and consistent eye exams is vital to protect long-term vision.
Why Inflammation Matters
Inflammation is the common factor linking autoimmune disorders and cataracts. Persistent inflammation triggers the release of cytokines, signaling molecules that affect how tissues repair and respond. In the eye, excessive cytokine activity can interfere with lens metabolism and protein balance.
Over time, these biochemical shifts cause the lens to lose its natural transparency. The once-clear structure begins to scatter light instead of focusing it, resulting in blurred vision, glare, and difficulty distinguishing colors.
While not every patient with autoimmune disease will develop cataracts, prolonged inflammation, repeated flare-ups, and certain medications significantly increase the likelihood.
Recognizing Early Symptoms
Cataracts associated with autoimmune diseases tend to develop gradually. Early symptoms are often subtle and may resemble other vision changes. Common signs include:
- Blurry or foggy vision
- Sensitivity to bright lights
- Difficulty seeing at night
- Fading or yellowing of colors
- Increased need for brighter lighting when reading
- Glare around headlights or lamps
If you experience these symptoms, scheduling an eye examination can help determine whether cataracts or another condition is responsible.
Diagnosis and Evaluation
Diagnosing cataracts in individuals with autoimmune disorders follows the same process as in the general population, but often includes closer attention to underlying inflammation.
Your eye doctor will typically perform:
- Visual Acuity Testing: Measures how well you can see at different distances.
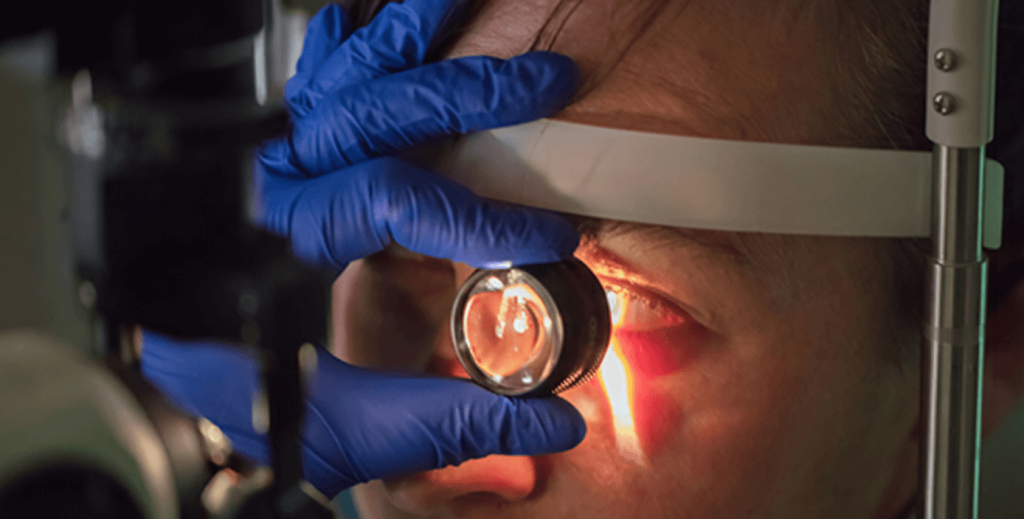
- Slit-Lamp Examination: Allows your doctor to examine your eye’s lens and surrounding structures in detail.
- Dilated Fundus Exam: Helps visualize the back of the eye and confirm the presence and severity of cataracts.
- Contrast Sensitivity Testing: Detects subtle vision changes that may occur before major clarity loss.
Patients with autoimmune diseases may also undergo additional imaging or lab work if inflammation is suspected in the ocular tissues.
Managing Cataracts in Autoimmune Patients
The good news is that cataracts can be safely treated regardless of their cause. Surgery remains the standard solution once cataracts begin to affect daily vision.
However, individuals with autoimmune disorders require a slightly more tailored approach. The focus is on minimizing inflammation before and after surgery to support a smooth recovery.
Preoperative Considerations
Your ophthalmologist will coordinate with your treating physician or rheumatologist to review your current medications and disease activity. If inflammation is active, surgery may be delayed until it stabilizes.
You may be prescribed anti-inflammatory medications before the procedure to keep your eyes calm. Close monitoring before and after surgery helps prevent flare-ups that could interfere with healing.
During Surgery
Cataract surgery is typically an outpatient procedure. It involves removing the cloudy lens and replacing it with a clear artificial lens. You’ll remain awake but comfortable during the procedure, and it usually takes less than an hour.
Your doctor will use advanced technology to minimize tissue disturbance, supporting a smoother recovery.
Recovery and Postoperative Care
After surgery, your ophthalmologist will prescribe eye drops to reduce inflammation and protect against infection. These are especially important for individuals with autoimmune conditions.
Follow-up appointments are essential to confirm proper healing. Any new discomfort, redness, or blurred vision should be reported immediately, as autoimmune-related inflammation can sometimes reactivate.
With consistent care, most patients achieve excellent visual outcomes.
Preventing or Slowing Cataract Formation
While cataracts cannot be fully prevented, certain steps can help reduce risk or delay progression, especially for those managing autoimmune conditions:
- Maintain Regular Eye Exams: Annual visits help identify early lens changes.
- Control Inflammation: Work closely with your healthcare team to manage autoimmune flare-ups.
- Use Medications Responsibly: Follow your doctor’s instructions regarding corticosteroids and ask about alternatives when possible.
- Protect Your Eyes from UV Light: Wear sunglasses outdoors to limit ultraviolet exposure.
- Maintain a Healthy Diet: Foods rich in antioxidants, like leafy greens and colorful fruits, support eye health.
- Monitor Blood Sugar Levels: For autoimmune conditions like Type 1 diabetes, glucose control plays a critical role.
By integrating these steps into your care routine, you can support your long-term vision health.
When to See Your Doctor
If you live with an autoimmune condition and notice any visual changes, it’s best to contact your eye doctor as soon as possible. Blurry or dim vision, increased glare, or new sensitivity to light may signal that cataracts are forming.
Even if your vision seems stable, regular exams are recommended. Detecting early lens changes allows your doctor to track progression and help you decide the right time for treatment.
Eye exams also provide an opportunity to assess for other conditions that can accompany autoimmune diseases, such as glaucoma or retinal inflammation.
The Connection Between Autoimmunity, Medication, and Cataracts
One of the most significant contributors to cataracts in autoimmune patients is corticosteroid therapy. These medications are highly effective at controlling inflammation but can alter the natural balance of lens proteins and fluids.
The risk of cataract formation depends on dosage, duration, and type of corticosteroid used. Oral steroids tend to have the most pronounced impact, but inhaled or topical forms can contribute as well.
Because steroids are often necessary to control disease activity, regular eye evaluations remain the best way to catch lens changes early. Your doctor can adjust your dosage or switch medications if cataract progression accelerates.
Living with an Autoimmune Condition and Protecting Vision
Managing an autoimmune disorder requires long-term care, but maintaining healthy vision is achievable. Proactive communication between your eye care specialist and other members of your medical team helps reduce complications and supports better outcomes.
Simple habits, like wearing protective eyewear outdoors, staying hydrated, and keeping inflammation under control, can go a long way in preserving lens clarity.
Remember, cataract surgery is both safe and highly successful. Most patients regain sharp vision and experience an improved quality of life after the procedure.
Summary
Autoimmune conditions such as rheumatoid arthritis, lupus, Sjögren’s syndrome, Type 1 diabetes, sarcoidosis, and others can contribute to cataract formation. The connection lies in chronic inflammation and the long-term use of corticosteroid medications.
Regular eye exams, careful medication management, and open communication between your medical specialists form the foundation for protecting your vision. If cataracts do develop, modern surgery provides a reliable and effective treatment option.
Ready to take the next step toward a clearer vision? Schedule a consultation with SuraVision today to discuss your options and learn more about Cataract Surgery. Call us at 713-730-2020 or book your appointment online!

